What is Diabetes?
Diabetes is very common. According to the National Diabetes Statistics Report 2020, 34.2 million people in the United States had diabetes in 2018. The percentage of the population with diabetes increases according to age, reaching 26.8% in adults aged 65 and older. Diabetes is a chronic (long-lasting) health condition that affects how your body turns food into energy. Most of the food you eat is broken down into sugar (also called glucose) and released into your bloodstream. When your blood sugar goes up, it signals your pancreas to release insulin. Insulin acts like a key in letting the blood sugar into your body’s cells for use as energy.
If you have diabetes, your body either doesn’t make enough insulin or can’t use the insulin it makes as well as it should. When there isn’t enough insulin or cells stop responding to insulin, too much blood sugar stays in your bloodstream. Over time, that can cause serious health problems, such as heart disease, vision loss, and alcoholic kidney disease. There isn’t a cure yet for diabetes, but losing weight, eating healthy food, and being active can really help. Taking medicine as needed, getting diabetes self-management education and support, and keeping health care appointments can also reduce the impact of diabetes on your life.


Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Mental Health Dual Diagnosis High-Quality Care at the We Level Up Treatment Centers Network.
Hotline (877) 378-4154Types of Diabetes
There are three main types of diabetes: type 1, type 2, and gestational diabetes (diabetes while pregnant).
Type 1 Diabetes
Type 1 diabetes is thought to be caused by an autoimmune reaction (the body attacks itself by mistake) that stops your body from making insulin. Approximately 5-10% of the people who have diabetes have type 1. Symptoms of type 1 diabetes often develop quickly. It’s usually diagnosed in children, teens, and young adults. If you have type 1 diabetes, you’ll need to take insulin every day to survive. Currently, no one knows how to prevent type 1 diabetes.
Type 2 Diabetes
With type 2 diabetes, your body doesn’t use insulin well and can’t keep blood sugar at normal levels. About 90-95% of people with diabetes have type 2. It develops over many years and is usually diagnosed in adults (but more and more in children, teens, and young adults). You may not notice any symptoms, so it’s important to get your blood sugar tested if you’re at risk. Type 2 diabetes can be prevented or delayed with healthy lifestyle changes, such as losing weight, eating healthy food, and being active.
Gestational Diabetes
Gestational diabetes develops in pregnant women who have never had diabetes. If you have gestational diabetes, your baby could be at higher risk for health problems. Gestational diabetes usually goes away after your baby is born but increases your risk for type 2 diabetes later in life. Your baby is more likely to have obesity as a child or teen, and more likely to develop type 2 diabetes later in life too.
Prediabetes
In the United States, 96 million adults—more than 1 in 3—have prediabetes. What’s more, more than 8 in 10 of them don’t know they have it. With prediabetes, blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes. Prediabetes raises your risk for type 2 diabetes, heart disease, and stroke. The good news is if you have prediabetes, a CDC-recognized lifestyle change program can help you take healthy steps to reverse it.
Alcohol and Diabetes Type 2
The hormone insulin, which is produced in the pancreas, is an important regulator of blood sugar levels. In people with diabetes, the pancreas does not produce sufficient insulin (type 1 diabetes) or the body does not respond appropriately to the insulin (type 2 diabetes).
Alcohol consumption by diabetics can worsen blood sugar control in those patients. For example, long-term alcohol use in well-nourished diabetics can result in excessive blood sugar levels. Conversely, long-term alcohol ingestion in diabetics who are not adequately nourished can lead to dangerously low blood sugar levels.
Heavy drinking, particularly in diabetics, also can cause the accumulation of certain acids in the blood that may result in severe health consequences. Finally, alcohol consumption can worsen diabetes-related medical complications, such as disturbances in fat metabolism, nerve damage, and eye disease.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug & Alcohol Rehab Centers Near You? Or Mental Health Support?
Even if you have failed previously, relapsed, or are in a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. Call us when you feel ready or want someone to speak to about therapy alternatives to change your life. Even if we cannot assist you, we will lead you wherever you can get support. There is no obligation. Call our hotline today.
FREE Addiction Hotline – Call 24/7
Alcoholism and Diabetes
Chronic use of alcohol (alcoholism) is considered to be a potential risk factor for the incidence of type 2 diabetes mellitus, which causes insulin resistance and pancreatic β-cell dysfunction that is a prerequisite for the development of diabetes [4].
Diabetes, especially type 2, causes dysregulation of various metabolic processes, which includes a defect in the insulin-mediated glucose function of adipocytes, and impaired insulin action in the liver.
Chronic heavy consumption deteriorates glucose tolerance and insulin resistance, and this may well be one of the mechanisms involved in the malignant effect of alcohol with regard to the development of diabetes.
Alcohol Interacts with Diabetes Medications
Most people who consume alcohol, whether in moderate or large quantities, also take medications, at least occasionally. As a result, many people ingest alcohol while the medication is present in their bodies or vice versa. A large number of medications—both those available only by prescription and those available over the counter (OTC)—have the potential to interact with alcohol. Those interactions can alter the metabolism or activity of the medication and/or alcohol metabolism, resulting in potentially serious medical consequences. For example, the sedative effects of both alcohol and sedative medications can enhance each other (i.e., the effects are additive), thereby seriously impairing a person’s ability to drive or operate other types of machinery.
Alcohol Can Cause Hypoglycemia
Unlike with many other aspects of diabetes and diet, the immediate risk with alcohol consumption is severe hypoglycemia or dangerously low blood sugar. This can be an emergency situation.
One reason for hypoglycemia with alcohol and diabetes type 2 is that alcohol can interfere with some diabetes medications, including sulfonylureas, meglitinides, and insulin. The result can be too much insulin action and a drop in blood sugar.
Another reason for hypoglycemia is that your liver is needed to metabolize alcohol, which takes its attention away from another duty: regulating blood sugar. The liver stores glycogen, a form of carbohydrate, and releases it to maintain blood sugar levels if they drop too much between meals. This mechanism is interrupted when you drink, and blood sugar can fall.
Hypoglycemia can also occur within 1 to 3 hours after drinking if you chose sugary mixed drinks or ate high-carbohydrate foods while drinking. This is known as reactive hypoglycemia because it happens as your body reacts to the sugar and other carbs by releasing more insulin.
Signs of hypoglycemia include shakiness, anxiety, confusion, dizziness, fatigue, and nausea. Headaches and seizures are also possible. A diabetic coma could result. Check your blood sugar if you have any of these symptoms. If you are unable to check your levels, treat it as though you know that you have hypoglycemia.
- Do not drink any more alcohol.
- If you have mild hypoglycemia with blood sugar 55-70 mg/dl, have 15 grams of carbohydrates and recheck your blood sugar in 15 minutes. Repeat until your number is higher than 70.
- If you have severe hypoglycemia with blood sugar less than 54 mg/dl, you may need to use injectable glucagon. You can get a prescription for this and carry it on your body. Let others know how to use it so they can administer it in case you are unconscious due to hypoglycemia.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline (877) 378-4154Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Diabetes and Alcohol Consumption
Individuals with diabetes should be especially cautious when it comes to alcohol consumption because alcohol can make some of the complications of diabetes worse. First of all, drinking alcohol affects the liver in doing its job of controlling blood sugar. Alcohol can also interact with some medications that are prescribed to individuals with diabetes. Even if you only rarely drink alcohol, talk with your healthcare provider about it so that he or she knows which medications are best for you.
Alcohol interacts with diabetes medications
- Alcohol consumption can cause blood glucose levels to rise or fall, depending on how much you drink. Some diabetes pills (including meglitinides and sulfonylureas) also lower blood glucose levels by stimulating the pancreas to make more insulin. Combining the blood-sugar-lowering effects of the medication with alcohol can lead to hypoglycemia or “insulin shock,” which is a medical emergency.
Alcohol prevents your liver from doing its job
- The main function of your liver is to store glycogen, which is then stored form of glucose so that you will have a source of glucose when you haven’t eaten. When you drink alcohol, your liver has to work to remove it from your blood instead of working to regulate blood sugar or blood glucose. For this reason, you should never drink alcohol when your blood glucose is already low.
Never drink alcohol on an empty stomach
- Food slows down the rate at which alcohol is absorbed into the bloodstream. Be sure to eat a meal or snack containing carbohydrates if you are going to drink alcohol.
Always test blood sugar before having an alcoholic beverage
- Alcohol impairs your liver’s ability to produce glucose, so be sure to know your blood glucose number before you drink an alcoholic beverage.
Alcohol can cause hypoglycemia
- Within a few minutes of drinking alcohol, and for up to 12 hours afterward, alcohol can cause your blood glucose level to drop. After consuming alcohol, always check your blood glucose level to make sure it is in the safe zone. If your blood glucose is low, eat a snack to bring it up.
You can save your life by drinking slowly
- Drinking too much alcohol can make you feel dizzy, sleepy, and disoriented—the same symptoms as hypoglycemia. Be sure to wear a bracelet that alerts people around you to the fact that you have diabetes so that if you start to behave like you are intoxicated they know that your symptoms could be caused by hypoglycemia. If you are hypoglycemic, you need food and/or glucose tablets to raise your blood glucose level.
You can save your life by knowing your limit
- Your healthcare provider will tell you how much alcohol is safe for you to drink. Depending on your health condition, that may mean no alcohol at all. In some cases, women with diabetes may have no more than one alcoholic beverage a day. Men should have no more than two.
Excessive Alcohol and Diabetes
Continuing to drink alcohol while struggling with diabetes can be detrimental to health. Alcohol can block the production of glucose by the liver, which can cause super low blood sugar. Symptoms of low blood sugar, or hypoglycemia, are often similar to the symptoms of alcohol consumption, making it hard to know the difference between the two issues. Both alcohol and low blood sugar can make a person have blurred vision and slurred speech, sleepy, and experience impaired cognitive abilities and coordination.
Excessive drinking can also damage the liver, which helps to filter toxins out of the body and process medications, which can then contribute to more side effects when diabetes is also present since diabetics may need to take medications to control the condition. The effects of alcohol can be unpredictable and lead to unsafe fluctuations in a person’s blood sugar that can continue for several hours after stopping drinking; this can be very dangerous for someone who struggles with diabetes and has unstable blood glucose levels already.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL (877) 378-4154End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Alcohol Addiction and Withdrawal Treatment
Detox is often considered the first stage of treatment. It will help you navigate the complicated process of alcohol withdrawal, but it doesn’t address patterns of thought and behavior that contribute to alcohol use. Various treatment approaches and settings can help provide the ongoing support necessary to maintain long-term sobriety after you complete detox.
Cravings are very common during detox and can be challenging to overcome. This often leads to relapse. Constant medical care provided during inpatient treatment helps prevent relapse. Clinicians can provide necessary medication and medical expertise to lessen cravings and the effects of alcohol withdrawals.
Medication-Assisted Treatments
Medication-Assisted Treatments (MAT) for alcohol use disorder and mental health disorder are commonly used in conjunction with one another. This includes the use of medications and other medical procedures. During your rehab, the staff from your treatment facility will help you identify what caused your addiction and teach you skills that will help you change your behavior patterns and challenge the negative thoughts that led to your addiction. Sometimes, the pressures and problems in your life lead you to rely on substances to help you forget about them momentarily.
Integrated Mental Health Care
Alcohol affects mental health, so people may use it to self-medicate undiagnosed disorders. Rehab centers typically provide mental health screenings, diagnoses, and integrated treatment for co-occurring disorders. In addition, holistic and therapeutic approaches are often used to treat recovering addicts with these conditions.
Behavioral Therapies
Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) can improve addicts’ behavior. CBT targets negative and maladaptive thought patterns as it promotes positive emotions and beliefs, while DBT helps clients address conflicting impulses so they can make healthy choices. Both therapies treat substance abuse and mental health disorders. Therapy also empowers clients to identify, avoid and mitigate cues that trigger drug cravings.
Individual and Group Counseling
Addiction and mental health counseling occur in both individual and group settings. One-on-one treatment sessions may address unresolved trauma, unconscious conflicts, and specific struggles, while group sessions often involve training in life skills, stress management, conflict resolution, and social connections. Group counseling also gives clients the chance to share their thoughts and experiences to develop social support, which is essential for lasting recovery. If you or someone you know is experiencing the effects of alcohol and diabetes type 2, it is crucial to intervene early. We Level Up NJ has addiction specialists that are standing by to help.

Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.
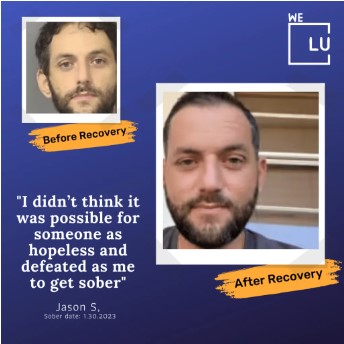


Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers various recovery programs at each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
Sources:
[1] NDSR – https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
[2] CDC – https://www.cdc.gov/diabetes/basics/diabetes.html
[3] NCBI – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6761899/
[4] NCBI – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3335891/
[5] NIAAA – https://pubs.niaaa.nih.gov/publications/arh23-1/40-54.pdf