Alcohol and Kidneys
Alcohol Liver Disease
Liver diseases make you more likely to experience discomfort or pain after alcohol consumption. This is particularly possible if your liver is affected by alcoholism. Alcohol liver damage can also affect blood flow to the kidneys and be less effective in filtering blood.
To treat liver diseases like alcoholic hepatitis and cirrhosis, your doctor may suggest you quit drinking alcohol, lose weight, and follow a healthy and nutritious diet. Some cases of liver disease may need medications or surgery. In addition, a liver transplant may be necessary in cases of liver failure.
Kidney Stones
Kidney stones may form because of alcohol-induced dehydration. Alcohol consumption and kidney stones may lead them to move quickly, increasing or contributing to kidney pain. It may be possible to treat small kidney stones by taking medication, drinking more water, or using home remedies.
Kidney Infection
A kidney infection is a type of urinary tract infection (UTI). It forms in the urethra or bladder and travels to one or both kidneys.
The condition and symptoms of a urinary tract infection may worsen after drinking alcohol. If you have a kidney infection, drink plenty of water and consult your doctor immediately.
You can use pain medication to relieve discomfort. Severe or recurring kidney infections may need surgery or hospitalization.
Dehydration
Alcohol features diuretic properties that lead you to urinate more frequently. This leads to dehydration, particularly with extreme alcohol consumption.
Alcohol affects the kidneys’ function to maintain electrolytes and water balance in the body. This results in damaged kidney function and increases the risk of forming kidney stones. Chronic dehydration leads you to a greater risk for these damaging effects.
Treat dehydration by drinking lost fluids and electrolytes, such as a sports drink with electrolytes and a carbohydrate solution. Avoid sugary beverages. In some cases, dehydration needs a visit to the doctor.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Mental Health Dual Diagnosis High-Quality Care at the We Level Up Treatment Centers Network.
Hotline (877) 378-4154Alcohol and Kidney Stones
Alcohol and kidney stones can both be serious health problems. However, it is possible to take action to reduce the risk of both. For kidney stones, staying hydrated is key, as drinking plenty of fluids can help to prevent kidney stones or other forms of urinary tract infections. Avoiding alcohol, or drinking responsibly, can help reduce the risk of alcohol-related problems such as cirrhosis of the liver. There are also treatments for alcohol and kidney stones, such as prescription medications and lifestyle modifications. It’s important to talk to a healthcare professional if you have any health concerns.
Kidney Stones and Alcohol Causation
Can alcohol cause kidney stones? And does alcohol make kidney stones worse? It has not been proven that drinking alcohol causes kidney stones. Alcohol can, however, dehydrate individuals, and dehydration has been linked to kidney stone development. Because of this, it is not advised to drink alcohol if you have kidney stones or are attempting to avoid getting them. In addition, dehydration, weight gain, and uric acid all play a factor.
Can drinking alcohol cause kidney stones? And does alcohol affect kidney stones? Although alcohol kidney stones may not be directly related, there are many reasons to limit your alcohol intake if you have kidney stones alcohol concerns.
Kidney stone and alcohol don’t go well together because kidney stones may be caused by dehydration, and alcohol can cause dehydration when taken.
Are Alcohol and Kidney Stones Connected?
If you have kidney stones, you may need to take steps such as avoiding high-oxalate foods, staying hydrated, and adding citrate to your diet. This can help to prevent stones or reduce the size of ones that may have already formed. For those who suffer from alcohol addiction, receiving professional help is important. Seeking treatment and engaging in activities such as support groups, therapy sessions, and comprehensive recovery plans are all useful steps one can take to overcome alcoholism. Additionally, lifestyle modifications such as engaging in regular exercise and eating healthy meals can also help one on their journey to sobriety.

Alcohol and Kidney Stones Symptoms
The surrounding areas of your kidneys may feel sore after alcohol consumption. This is the area under your ribcage, at the back of your abdomen, on both sides of your spine. This pain may be felt as a sharp, sudden, stabbing pain or more of a dull ache. It may be mild or severe and can be felt on one or both sides of the body.
The pain in your kidneys may be felt in the upper or lower back or between the buttocks and lower ribs. The pain may be felt immediately after drinking alcohol or after you’ve quit drinking. Sometimes it gets worse at night.
Other symptoms include:
- Vomiting
- Nausea
- Painful urination
- Blood in the urine
- Loss of appetite
- Trouble sleeping
- Headaches
- Fatigue
- Fever
- Chills
How Alcohol Affects Your Kidneys
Alcohol consumption affects many parts of your body, including your kidneys. A small amount of alcohol—one or two drinks now and then—usually has no severe effects. However, excessive drinking–more than four drinks daily—can affect your health and worsen kidney disease. When experts talk about one drink, they are talking about one 12–ounce bottle of beer, one glass of wine, or one ounce (one shot) of “hard liquor.” When a person drinks too much, alcoholic kidney stones may form.
Binge drinking harms the kidney, leading to acute kidney failure. A sudden drop in kidney function is called acute kidney failure. This often goes away but can occasionally lead to lasting kidney damage. Regularly drinking too much too often can also damage the kidneys. However, the damage occurs more slowly. Regular heavy drinking has been found to double the risk of chronic kidney disease.
A higher risk of kidney problems has been found for heavy drinkers who smoke. Heavy drinker smokers have about five times the chance of developing chronic kidney disease than people who don’t smoke or drink alcohol excessively. When taken too much kidney stone alcohol may result from it.
The kidneys have an essential job as a filter for toxic substances. One of these substances is alcohol. The kidneys of heavy drinkers have to work harder. Alcohol causes changes in the role of the kidneys and makes them less able to filter the blood.
Alcohol also affects the capacity to control fluid and electrolytes in the body. When alcohol dehydrates the body, the drying effect can impact the normal operation of cells and organs, including the kidneys. In addition, alcohol can disrupt hormones that affect kidney function.
Effects on Body Fluid Volume and Blood Pressure
Excessive drinking can also affect your blood pressure. Individuals who consume too much alcohol are more likely to have high blood pressure. And medications for high blood pressure can have harmful interactions with alcohol. High blood pressure is a typical cause of kidney disease.
More than two drinks a day can increase your chance of developing high blood pressure. In addition, drinking alcohol in these amounts is a risk factor for developing a sign of kidney disease protein in the urine (albuminuria).
By promoting liver disease, chronic drinking adds to the kidney’s job. The blood flow rate to the kidneys is usually kept at a certain level so that the kidney can filter the blood well. Established liver disease impairs this critical balancing act. Most patients in the United States diagnosed with liver disease, and associated kidney dysfunction are alcohol-dependent.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug & Alcohol Rehab Centers Near You? Or Mental Health Support?
Even if you have failed previously, relapsed, or are in a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. Call us when you feel ready or want someone to speak to about therapy alternatives to change your life. Even if we cannot assist you, we will lead you wherever you can get support. There is no obligation. Call our hotline today.
FREE Addiction Hotline – Call 24/7How Much Alcohol is Too Much?
It’s best to first check with your renal dietitian or nephrologist to find out if alcohol is safe for you. If you can drink alcohol safely, your healthcare team will advise you on the types and amounts that are right for you. Once alcohol is taken excessively, kidney stones alcoholism may result from it.
Alcohol has no nutritional benefit, but it does have calories that can add up quickly. Take this into consideration when planning your daily menus. Some medicines, both prescription and over-the-counter, may interact with alcohol. and cause the medication not to work correctly.
Other medicines may cause your blood alcohol level to rise. Check drug labels and ask your pharmacist or doctor to review your medications to make sure alcohol will not be harmful to your prescription. Does Alcohol Help With Kidney Stones? Read more to find out.
Safe Levels of Drinking
The federal government’s Dietary Guidelines for Americans defines moderate drinking as:
- One drink per day for women and older people
- Two drinks per day for men
The limits are different for men and women because men usually weigh more, and alcohol is processed differently by the sexes. Women tend to have a stronger reaction to alcohol. One reason is that women have less water in their bodies, so alcohol becomes more concentrated. The risk for alcohol-related diseases is also higher in women than in men.
What is the best alcohol to drink with kidney stones? Although it is not sure what the best alcohol for kidney stones or worst alcohol for kidney stones is, all should be avoided or taken in moderation.
The following count as one drink, and each contains the same amount of alcohol:
- 12 ounces of beer or wine cooler
- 5 ounces of wine
- 1.5 ounces of 80-proof distilled spirits (whiskey, bourbon, scotch, vodka, gin, tequila, rum)
Does Alcohol Cause Kidney Stones?
Does alcohol help kidney stones? Alcohol consumption in moderation may prevent alcoholism kidney stones, according to a few small studies. The cause of this is unknown. However, it might be because beer is a diuretic that promotes urination. In turn, urination can help in flushing out minor kidney stones to prevent larger ones from forming.
When a health care provider refers to drinking in moderation, they typically imply no more than one drink for women and two for men per day. For beer or wine, a serving size would be about 12 ounces. Generally, kidney stones drinking alcohol won’t improve your condition, so it is best to avoid alcohol completely.
Can you drink alcohol with a kidney stone? While drinking enough fluids when you have kidney stones is important, drinking alcohol with kidney stones is not recommended. This is due to how dehydrating alcohol is. Dehydration might make you retain water and urinate less, making it more difficult to pass any existing stones. When facing alcoholism and kidney stones, it is best to seek attention from a medical professional to help you.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline (877) 378-4154Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Long-Term Alcohol Effects on the Kidneys
Your kidneys are a pair of organs that perform many essential bodily functions and regulate pH, produce hormones, and excrete wastes and toxins, such as alcohol. Drinking excessively can cause your kidneys to decrease their ability to filter your blood.
In addition, your kidneys also ensure your body’s hydration. Consuming alcohol dehydrates your body, which can have negative effects on the function of your kidneys and other vital organs.
Excessive alcohol use can also lead to high blood pressure, increasing your risk of developing kidney disease. After you drink an alcoholic beverage, your body experiences an acute spike in blood pressure for up to two hours. Over time, alcohol use can lead to a sustained rise in blood pressure.

Alcohol and Kidney Failure
Binge drinking has harmful effects on the kidney that can even lead to acute kidney failure. A sudden drop in kidney function is called acute kidney failure. Alcohol causing kidney stones may result from the side effects worsening when it is taken too much.
What is Kidney Failure?
Kidney failure means that 85-90% of your kidney function is gone, and they don’t work well enough to keep you alive. There is no cure for kidney failure, but it is possible to live a long life with treatment. Having kidney failure is not a death sentence; people with kidney failure live active lives and continue to do the things they love.
What Causes Kidney Failure?
High blood pressure and diabetes are the two most common causes of kidney failure. They can also become damaged from physical injury, diseases, or other disorders.
What Happens When Kidneys Fail?
Kidney failure does not happen overnight. It is the result of a gradual loss of kidney function. Some people do not even know they have kidney disease until their kidneys fail. Why not? Because people with early kidney disease may not have any symptoms. Symptoms usually show up later in the progression of the disease and may include:
- Trouble sleeping
- Poor appetite
- Weakness
- Tiredness
- Itching
- Weight loss
- Muscle cramps (especially in the legs)
- Swelling of your feet or ankles
- Anemia (a low blood count)
- Trouble sleeping
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL (877) 378-4154End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.

Alcohol and Kidney Stones Treatment
The CDC warns that binge drinking can cause acute kidney failure, but the damage can often be reversed if you stop drinking and allow your kidneys time to heal. This recovery timeline can vary depending on how long and much you drank.
Some of the damage can be irreversible, however. Regular heavy drinking doubles your risk for chronic kidney disease. This risk quadruples if you also smoke. Alcohol and kidneys have direct connections. Alcohol can raise your blood pressure, and heavy drinking can cause chronic high blood pressure. This is another risk factor for kidney disease.
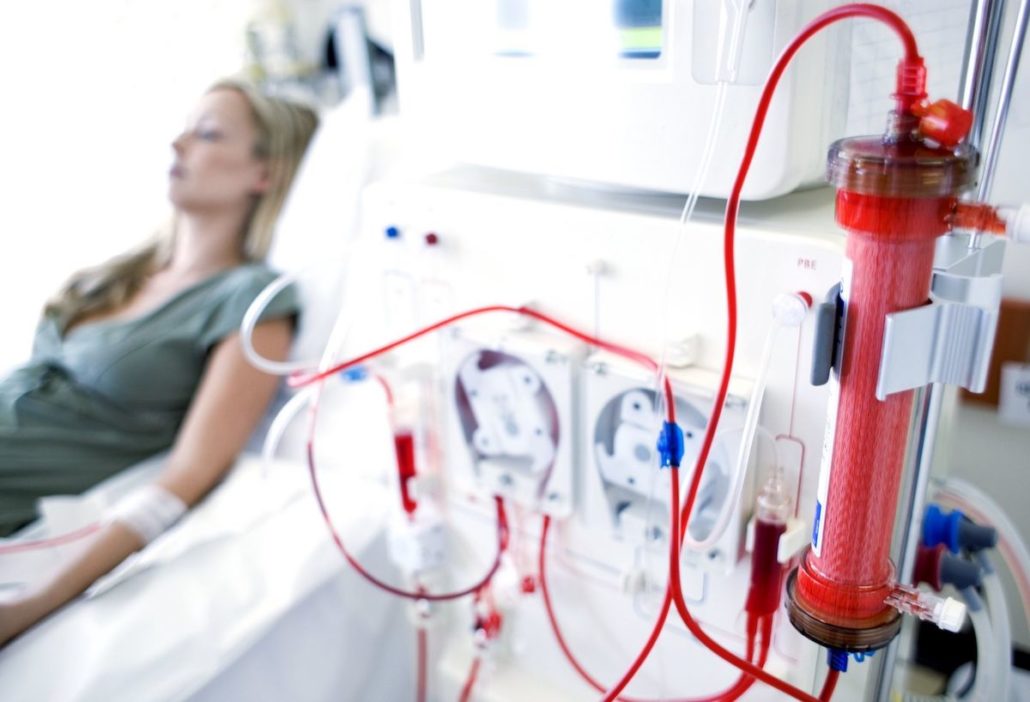
Kidney disease can lead to kidney failure. You may then need to endure regular kidney dialysis to filter your blood and keep things properly balanced or undergo a kidney transplant. Heavy drinking can make it hard for you to qualify for a kidney transplant.
Reducing the amount of alcohol you drink can positively impact your body and brain and allow your kidneys a chance to be healthy. Get help to stop heavy drinking and give your kidneys the best chance of a full recovery.
We Level Up NJ provides proper care with round-the-clock medical staff to assist your recovery through a medically-assisted detox program. Reclaim your life, and call to speak with a knowledgeable treatment specialist. Our counselors know what you are going through and will answer any of your questions.
Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.



Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers various recovery programs at each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews
We’ll Call You
FAQs
Does alcohol cause kidney stones? And does drinking alcohol cause kidney stones?
Even though kidney stones and alcohol aren’t directly related, alcohol can cause dehydration and may lead to kidney stone formation.
Does drinking alcohol help with kidney stones?
No, alcohol does not help with kidney stones. On the other hand, it may worsen because alcohol can cause dehydration.
Is alcohol bad for kidney stones? And can you get kidney stones from drinking alcohol?
Yes, because drinking excessive alcohol frequently increases the risk of kidney stones substantially.
Can you get kidney stones from alcohol?
Alcohol can cause kidney stones due to its high concentration of purines. Purines are chemical compounds that can lead to uric acid kidney stones.
Can I drink alcohol with kidney stones?
If you have kidney stones, drinking alcohol won’t help as it will make you feel dehydrated, and kidney stones may worsen.
Can alcohol give you kidney stones? and can alcohol trigger kidney stones?
While kidney stones and alcohol are not related, drinking alcohol excessively may result in kidney stones forming.
Can you drink alcohol while passing a kidney stone?
Although alcohol makes you urine more frequently, it can also dehydrate you. Alcohol and passing kidney stones can make the experience more painful and make the stone more likely to get stuck in your urinary tract system.
Is alcohol good for kidney stones?
In most cases, taking any alcohol is not recommended if you have kidney stones.
Can you take alcohol after kidney stone surgery?
Drinking alcohol after kidney stone surgery is generally not recommended since it will not help in any way.