What is Alcoholic Steatohepatitis?
Alcoholic Steatohepatitis is one of the alcohol liver damage diseases that can affect the liver as a result of long-term alcohol abuse. It is often chronic, progressive, and very lethal. The usual thing that occurs to the liver is fibrosis (scarring and thickening) [1]. In very severe cases, the condition can advance to a point where death (necrosis) occurs to liver tissues. All of these are caused by the excessive consumption of alcohol over a prolonged time. If you consume more than 60 ml of alcohol daily as a man or 40 ml as a woman, then you are at risk. Consuming more than those amounts is toxic and would end up damaging your liver which could eventually lead to alcoholic cirrhosis.
The timespan of consumption is also very important. The risks of alcohol-induced liver damage rise higher if you consume excess amounts of alcohol regularly for at least five years. Meanwhile, men can metabolize more alcohol than women. That is why the safe level for women is quite lower than for men. Women have more proneness to the disease than men. Genetic factors also seem to play a role in how susceptible a person is. Some other factors that may predispose a person to alcoholic steatohepatitis include nutrition existent chronic hepatitis (either B or C, among many other factors.


Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Mental Health Dual Diagnosis High-Quality Care at the We Level Up Treatment Centers Network.
Hotline (877) 378-4154Alcoholic Steatohepatitis Diagnosis
The liver biopsy can confirm the etiology of alcoholic steatohepatitis (ASH) and assess structural alterations of cells, their organelles, as well as inflammatory activity. Three histological stages of ALD are simple steatosis, ASH, and chronic hepatitis with hepatic fibrosis or cirrhosis. These latter stages may also be associated with a number of cellular and histological changes, including the presence of Mallory’s hyaline, megamitochondria, or perivenular and perisinusoidal fibrosis. Genetic polymorphisms of ethanol metabolizing enzymes such as cytochrome p450 (CYP) 2E1 activation may change the severity of alcoholic steatohepatitis (ASH) [2].
The classical clinical syndrome of alcoholic steatohepatitis (ASH) consists of jaundice, varying degrees of hepatic failure, abdominal distress, fever, and leukocytosis, although patients with the histological features of the entity may be asymptomatic and anicteric. The syndrome appears in patients who have been consuming excessive amounts of alcohol for periods of 1–5 years or more. Factors that affect the development of liver injury include the dose, duration, and type of alcohol consumption, drinking patterns, sex, age, ethnicity, as well as associated risk factors such as obesity, iron overload, concomitant infections, and genetics.
Alcoholic Steatohepatitis Pathology Outlines
Steatosis is defined as the accumulation of lipid droplets in the hepatocyte cytoplasm. The term “fatty degeneration” has been used when > 5% of hepatocytes show steatosis while the fatty liver is the term described when > 50% of hepatocytes show steatosis. In ALD the steatosis is usually macrovesicular or mixed microvesicular and macrovesicular.

It may begin with small droplets of fat in the cytoplasm (microvesicular), which later enlarge to large fat droplets (macrovesicular), which push the nucleus to the periphery. Macrovesicular fat droplets can coalesce to form fat cysts (large irregular extracellular fat vacuole). Continuing accumulation of fat may lead to rupture of the fat cyst with a histiocytic reaction or lipogranuloma [3].
Steatohepatitis indicates evidence of hepatic injury accompanying steatosis. The injury may be seen in the form of hepatocyte ballooning, neutrophil-rich inflammation in the lobular parenchyma. Ballooning degeneration of hepatocytes is the predominant mode of cellular injury in alcoholic hepatitis.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug & Alcohol Rehab Centers Near You? Or Mental Health Support?
Even if you have failed previously, relapsed, or are in a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. Call us when you feel ready or want someone to speak to about therapy alternatives to change your life. Even if we cannot assist you, we will lead you wherever you can get support. There is no obligation. Call our hotline today.
FREE Addiction Hotline – Call 24/7Alcoholic Steatohepatitis Symptoms
Symptoms usually become apparent in patients during their 30s or 40s; severe problems appear about a decade later. Most people don’t show any symptoms of alcoholic steatohepatitis. An abnormal liver blood test result may cause a red flag, so the doctor may run more tests to see what’s going on. Whether it’s alcoholic or non-alcoholic steatohepatitis, there may be some symptoms. As the disease progresses, more common symptoms may include:
- Nausea
- Weight loss
- Jaundice (the yellowing of eyes and skin)
- Fatigue
- Enlarged liver resulting in tender, painful abdomen
To determine if you have alcoholic steatohepatitis, typically, a liver biopsy will be performed. To see how far along the progression is, an ultrasound, CT scan, or MRI may be performed. Your doctor will likely look at your medical history and inquire about your drinking habits. If alcohol intake is limited, it could be nonalcoholic fatty liver disease.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline (877) 378-4154Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Causes and Risk Factors
To effectively cope with the problem, it is necessary to have an idea of both the disease itself and the sources that generate it. This pathology is an inflammation in the liver tissues that occurs against the background of the degeneration of the liver fat cells. Physicians divide into several types, which cause various pathologies. Causes of steatohepatitis.
- Alcoholic genesis. Almost every third person who abuses alcoholic beverages can observe the development of this deviation.
- Metabolic genesis – pathology based on disturbances in metabolic processes.
- Excessively large body weight.
- Deficiency of protein.
- Deficiency of insulin in the body, causing diabetes.
- Rapid weight loss.
- The hunger strike.
- Failure in lipid (fat) metabolism – dyslipidemia.
- Complete replacement of the patient’s natural nutrition by parenteral food intake (bypassing the digestive organs). Primarily this is an intravenous route.
- Continuous and repeated administration of glucose into the vein.
- Medicinal trace of the disease. A number of drugs can cause poisoning with chemical compounds (intoxication), as well as fatty infiltration, which is due to increased accumulation of lipid constituents in the liver cells. Such consequences can be observed after taking some medicines:
- Cytostatics that block the cell’s ability to divide.
- Glucocorticoids, directly affecting the human hormonal background.
- A number of antibiotic drugs.
- Non-steroidal anti-inflammatory drugs (NSAIDs) used as analgesics, anti-inflammatory and antipyretic agents.
- Provoke this deviation is also capable of surgical intervention, performed on the organs of the gastrointestinal tract, especially in the case of partial removal of the small intestine.
- The reason for degeneration is diverticulosis, a deviation resulting from the formation of a sacciform appearance of the wall of the small intestine. At the same time there is an increased increase in the intestine of a colony of pathogenic microorganisms.
- Wilson-Konovalov’s pathology, associated with a change in the normal exchange of copper.
- And a number of other factors. All sources of modern medicine are not yet known for certain.
Alcoholic Steatohepatitis Treatment
The liver is an incredible organ and may be able to reverse a good bit of the damage with its self-healing capabilities. However, if the disease has progressed into the final stages of liver disease, the chances of reversing the damage decrease significantly.
Abstaining from drinking all forms of alcohol is the first step to managing alcoholic steatohepatitis. Your physician may refer you to an alcohol recovery program if you’re struggling with quitting on your own.
To date, there are no medications that specifically treat this disease. To manage symptoms for both alcoholic and nonalcoholic fatty liver disease, physicians recommend:
- A healthy diet supplemented with vitamin B-12.
- To combat inflammation, corticosteroids may be prescribed to reduce the swelling.
- If obesity is an issue, weight loss may help reduce inflammation and fat in the liver.
- Regular exercise.
The medications people use when they have alcoholic steatohepatitis are to manage the symptoms and complications. For instance:
- Corticosteroids to reduce inflammation
- Antibiotics and probiotics for infections
- Other medications that target the pathway of inflammation
However, there are ongoing clinical trials on the efficiency of stem-cell therapy. Most of the management routines for alcoholic steatohepatitis are lifestyle amendments.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL (877) 378-4154End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Alcohol Abuse Treatment
Alcoholic steatohepatitis is a progressive disease that can ultimately lead to death. If you’re a moderate to heavy drinker, it’s best if you stop drinking entirely. If you cannot quit on your own, reach out for help. If the disease leads to alcoholic cirrhosis, your physician may treat it with various medications or surgery. If the liver starts to fail, there is the option of having a liver transplant.
The goal of alcoholic steatohepatitis treatment is to restore some or all normal functioning to the liver. Abstinence from alcohol can have a great effect on survival even in people with alcoholic steatohepatitis. However, if you have alcoholic steatohepatitis and do not stop drinking, no medical or surgical treatment can prevent liver failure. Thus, the treatment for alcohol-related liver disease and treatment for an alcohol use disorder go hand in hand.
The first step in treatment is to help the individual stop drinking. This may involve an inpatient alcohol treatment program. Sometimes diet changes are advised, too. The liver is often able to fix some of the damage caused by alcohol so you can live a normal life.
Medically Assisted Detox
Usually, the first step in inpatient alcohol treatment is medically assisted detox. Doctors and addiction specialists monitor clients’ vital signs while alcohol exit the system. Depending on the type of substance a person is detoxing from, alcohol withdrawal symptoms may differ.
Cravings are very common during detox and can be challenging to overcome. This often leads to relapse. Constant medical care provided during inpatient treatment helps prevent relapse. Clinicians can provide necessary medication and medical expertise to lessen cravings and withdrawals.
Medication-Assisted Treatments
Medication-Assisted Treatments (MAT) for alcohol use disorder and liver disease are commonly used in conjunction with one another. This includes the use of medications and other medical procedures. Typically, individuals undergoing alcohol withdrawal management are administered benzodiazepines under the supervision of an addiction medicine physician, whereas steroids are often used to deal with inflammation of the liver that is associated with alcoholic-related liver disease.
During your rehab, the staff from your treatment facility will help you identify what caused your addiction and teach you skills that will help you change your behavior patterns and challenge the negative thoughts that led to your addiction. Sometimes, the pressures and problems in your life lead you to rely on substances to help you forget about them momentarily.
Integrated Mental Health Care
Alcohol affects mental health, so people may use it to self-medicate undiagnosed disorders. Rehab centers typically provide mental health screenings, diagnoses, and integrated treatment for co-occurring disorders. In addition, holistic and therapeutic approaches are often used to treat recovering addicts with these conditions.
Behavioral Therapies
Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) can improve addicts’ behavior. CBT targets negative and maladaptive thought patterns as it promotes positive emotions and beliefs, while DBT helps clients address conflicting impulses so they can make healthy choices. Both therapies treat substance abuse and mental health disorders. Therapy also empowers clients to identify, avoid and mitigate cues that trigger drug cravings.
Individual and Group Counseling
Addiction and mental health counseling occur in both individual and group settings. One-on-one treatment sessions may address unresolved trauma, unconscious conflicts, and specific struggles, while group sessions often involve training in life skills, stress management, conflict resolution, and social connections. Group counseling also gives clients the chance to share their thoughts and experiences to develop social support, which is essential for lasting recovery.
Please, do not try to detox on your own because the detox process can be painful and difficult without medical assistance. It’s hard enough that you are struggling with liver disease. If you or someone you know regularly exceeds these recommended daily limits or is experiencing alcoholic steatohepatitis it is important to intervene early. We Level Up NJ has addiction specialists that are standing by to help.

Experience Transformative Recovery at the We Level Up Treatment Center.
See our authentic success stories. Get inspired. Get the help you deserve.
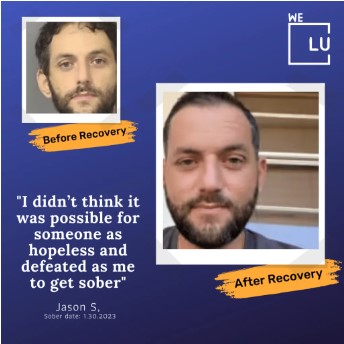


Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up treatment center network delivers various recovery programs at each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 5-Star Reviews